Cynata Therapeutics Limited, an Australian stem cell and regenerative medicine company, has announced the results of a preclinical trial in which it tests its Cymerus mesenchymal stem cell treatment in a preclinical heart attack model.
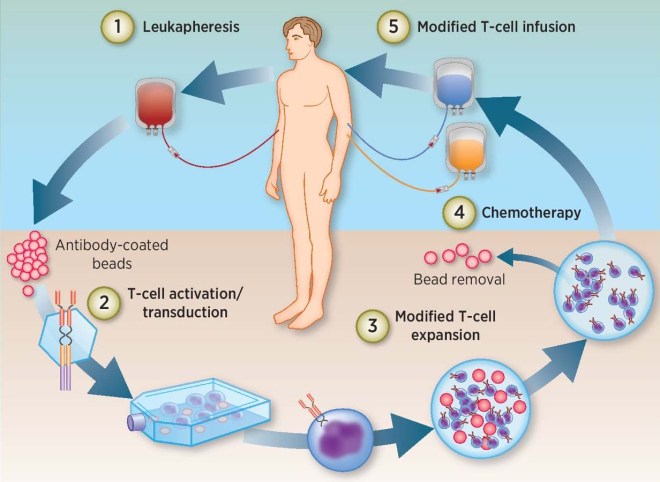
Cynata uses induced pluripotent stem cell technology to make large numbers of mesenchymal stem cells for therapeutic treatments. To review, induced pluripotent stem cells (iPSCs) are made from body cells by means of genetic engineering and cell culture techniques. Briefly, four different genes – OCT4, KLF4, SOX2, and c-MYC – are transfected into bodily cells. Transient expression of these genes in regular body cells drives a small proportion of them (0.1%-0.5%) to undergo dedifferentiation into developmentally immature cells that resemble embryonic stem cells. These embryonic stem cell-like cells, or iPSCs, will outgrow the other cells and can be successfully cultured in cell culture systems. Once purified, cloned, and established as a viable cell line, the iPSC cell line can be grown to large numbers and differentiated into specific cell types.
Cynata has differentiated iPSCs derived from cells provided a healthy donor to make a recently identified precursor cell, known as a mesenchymoangioblast (MCA). MCAs were first identified by Professor Igor Slukvin and his coworker from the University of Wisconsin-Madison. MCAs are early clonal mesoendodermal precursor cells that are the common precursor for both mesenchymal stem cells (MSCs) and endothelial cells, which are the main component of blood vessels. MCAs can also differentiate into pericytes and smooth muscle cells.
By making MCAs from iPSCs, Cynata seeks to overcome some of the largest hurdles for adult stem cell-based treatments, those being the dependence on donors for a steady supply of stem cells, the extensive variability of donated adult stem cells, the contamination of isolated adult stem cells with other cell types that do not have established therapeutic activities, and, probably most importantly, the limited scalability of stem cells from donors. Thus, in principle, Cynata’s Cymerus technology incorporates iPSC-derived MCA, which are used to make MCA-derived MSCs. This platform can potentially address the shortcomings of adult stem cell-based treatments, since iPSCs can proliferate indefinitely, and MCAs themselves can expand into extremely large quantities of MSCs. To quote the Cyanata web site; “Cynata should be able to manufacture all of the MCAs that it will ever need from a single Master Cell Bank of iPSCs – derived from a single donor.”
This most recent experiment was conducted by James Chong, Associate Professor at the Westmead Institute for Medical Research in Sydney, Australia, and colleagues. Chong and his coworkers induced heart attacks in three groups of rats (15 groups per group) and treated them four days later. All the laboratory animals were assessed for 28 days after the heart attack (I wish they had observed them for longer periods of time). The rat groups consisted of three treatment groups: Group 1 received infusions of Cymerus MSCs, which were derived from iPSC-derived MCAs; Group 2 received MSCs from bone marrow; Group 3 was a placebo group that received infusions of buffer. All post-heart attack assessments were performed in a blinded manner, which simply means that the staff conducting the assessments had no idea which treatment the animal they tested had received.
The results of this study were rather encouraging. The first category examined was “fractional shortening,” which is an estimate of the ability of the heart to contract effectively. Improvements in fractional shortening is indicative of recovery of the pumping function of the heart after a heart attack. Treatment with Cynata’s Cymerus MSCs resulted in an improvement in fractional shortening 28 days after the heart attack. Statistical comparisons showed that the Cymerus MSC-induced improvements were better than those observed in the placebo group (p=0.013) and the BM-MSC group (p=0.003).
The next assessment examined the effects of these treatments on left ventricular end-systolic diameter (LVESD). If, after a heart attack, the LVESD values are higher, then the heart is not contracting well. However, reduced LVESD values are associated with improved cardiac function and correlated quite well with a reduced risk of further cardiac events. In this study, LVESD was lower in the Cymerus MSC group compared to those rats that had been treated with the placebo (p=0.054) and bone marrow-derived MSCs (p<0.001).
Finally, Chong and his gang examined the scar size as a proportion of the left ventricle size. For all three groups, there were no statistically significant differences between groups when it came to scar size as a proportion of the size of the left ventricle. It is possible that 28 weeks is far too short a time for the stem cells to produce any reduction in the size of the cardiac scar. Therefore, further assessments of scar are ongoing.
To summarize, the Cymerus MSC treatments improved recovery of cardiac function post heart attack and reduced left ventricular end-systolic diameter (LVESD) compared to either placebo or bone marrow-derived MSCs, and further demonstrates the broad applicability of the Cymerus cell-manufacturing platform for clinical treatments.
In response to these positive results, Cynata’s Vice President of Product Development, Dr. Kilian Kelly said: “These very encouraging results add to a growing body of evidence showing that Cymerus MSCs may have an important role to play in the treatment of a wide range of diseases. There is still a huge unmet medical need associated with heart attacks, which cause over 8,000 deaths and more than 50,000 hospitalizations each year in Australia alone. We are optimistic about the potential benefits that Cymerus MSCs could bring to patients who experience these life-changing events.”