Umbilical cord blood infusions save the lives of many children and adults each year. Umbilical cord blood contains hematopoietic stem cells (HSCs) that can replace those lost to anticancer treatments, chemicals, or bone marrow collapse. However, despite their advantages for transplantation, the clinical use of umbilical cord blood is limited by the fact that HSCs in cord blood are found only in small numbers.
Small molecules that enhance hematopoietic stem and progenitor cell (HSPC) expansion in culture have been identified (see Boitano, A. E. et al. Science 329, 1345–1348 (2010), and Fares, I. et al. Science 345, 1509–1512 (2014). Unfortunately, the mechanisms of action or the nature of the pathways they impinge on are poorly understood.
Now a research team from McMaster University’s Stem Cell and Cancer Research Institute have discovered a key protein in the HSC/HSPC regenerative signaling pathway.
Kristin J. Hope and her team have elucidated the role of a protein called Musashi-2 in the function and development of HSCs.
Dr. Hope says that this discovery could help the tens of thousands of patients who suffer from blood-based disorders, including leukemia, lymphoma, aplastic anemia, sickle-cell disease, and more.
“We’ve really shone a light on the way these stem cells work,” she said. “We now understand how they operate at a completely new level, and that provides us with a serious advantage in determining how to maximize these stem cells in therapeutics. With this newfound ability to control over the regeneration of these cells, more people will be able to get the treatment they need.”
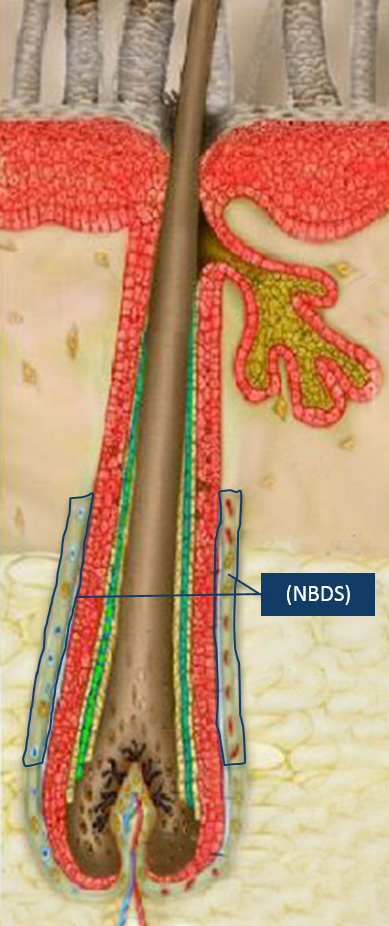
Only about five percent of all umbilical cord blood samples contain enough HSCs for a transplant, which is unfortunate because umbilical cord blood is less likely to be rejected by the immune system, because of the immaturity of the cells, and is also rather abundant.
Growing HSCs in culture is a possibility, but this remains a somewhat poorly understood and ill-defined procedure.
Musashi-2 is an RNA-binding protein in cells and was actually named for the Japanese samurai who fought using two swords.
In collaboration with researchers in Dr. Gene Yeo’s lab at the University of California San Diego, Dr. Hope’s lab has found that the Musashi-2 protein plays a pivotal role in controlling stem cell production in human cord blood HSCs. When Musashi-2 levels in HSCs are the knocked down, the cod blood HSCs were no longer able to regenerate the blood system. Conversely, when the levels of Musashi-2 were increased, the number of HSCs in the cord blood sample increased significantly.
The Hope’s group new discovery has identified a new way to tightly control on the development of HSCs. Essentially, Hope and her colleagues have discovered a new way to make more cord blood stem cells in a dish.
In the past, attempts to control HSC function and development has been approached at the level of transcriptional factors. The Hope lab’s approach of directing stem cell function through manipulation of an RNA-binding protein is somewhat novel, and represents a paradigm shift in the way we think about stem cell biology.
“This discovery really highlights the underappreciated role that RNA-binding protein-mediated control has on the properties of stemness in the blood system,” explained Dr. Hope.
This paradigm shift provides new targets for pharmaceuticals that may be able to expand these cells in a safe and targeted manner.
These findings represent an important step forward in surmounting the obstacles associated with stem cell transplants. According to Dr. Hope, the ability to increase the number of available cord blood stem cells has the potential to “mitigate a lot of the problems that arise post-transplantation.” Elaborating further, Dr. Hope explained that stem cells from cord blood are a “safer and more efficient transplant product,” and detailed how their use could reduce the number of patient follow-up visits and treatments required post-transplantation. Streamlining the transplantation process could help to alleviate the stress on the healthcare system and open up space for more transplant patients.