Bone marrow contains a treasure trove of stem cells. Hematopoietic stem cells make all the blood cells, mesenchymal stem cells make bone, cartilage and fat, and endothelial progenitor cells make the endothelial cells that line blood vessels. There are almost certainly other types of stem cells in bone marrow, but one stem cell population, the very small embryonic-like stem cells (VSELs), took a large hit this year when Irving Weissman and his co-workers at Stanford were unable to confirm their existence. Until this is resolved, the existence of VSELs must remain a question mark.
With all this comes an interesting paper from the laboratory of Muhammad Ashraf at the University of Cincinnati Medical Center in the American Journal of Physiology, Heart Circulation Physiology (August 30, 2013) that reports the existence of “small juvenile stem cells” in the bone marrow of aged rats. These cells have healing capabilities and anti-aging abilities.
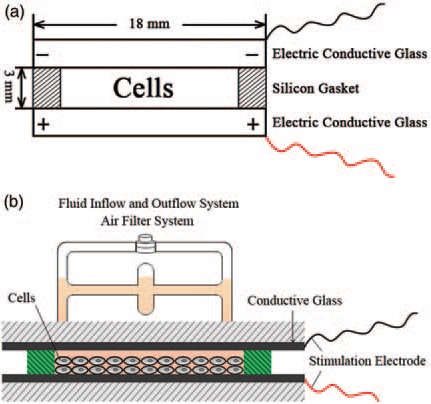
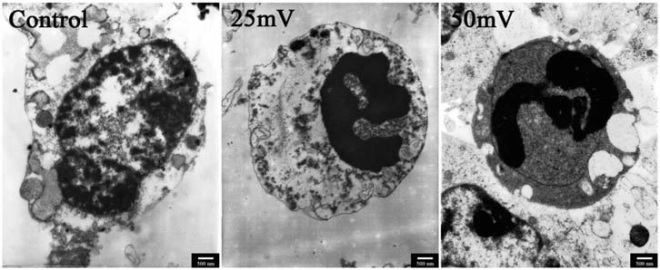
To begin, Ashraf and others isolated bone marrow from rats and spooned it into culture dishes with a rather standard cell culture medium (DMEM supplemented with calf serum and low glucose). Cells that did not adhere to the culture dish were discarded (hematopoietic stem cells do not adhere) and the remaining cells were grown in fresh culture medium for 6-10 days. The cells had a spindle-shape to them and they were passaged for no more than 6 times. Then they were grown on culture wells that had 3 micron pores. This way, only the small cells could migrate to the other side of the pore. After one day, the cells that had moved through the pores were collected and grown or another 10-15 days.
Thus, these cells were definitely small. Further characterization showed that they expressed some, but not all of the markers of mesenchymal stem cells, suggesting that these small cells are of a different sort than mesenchymal stem cells. Then Ashraf and his colleagues measured the growth of these small bone marrow stem cells and found that they grew quickly and steadily. Even more telling, the small bone marrow stem cells from older rats grew just as fast and the small bone marrow stem cells from young mice. Thus Ashraf and his group named these cells “small juvenile stem cells” or SJSCs.
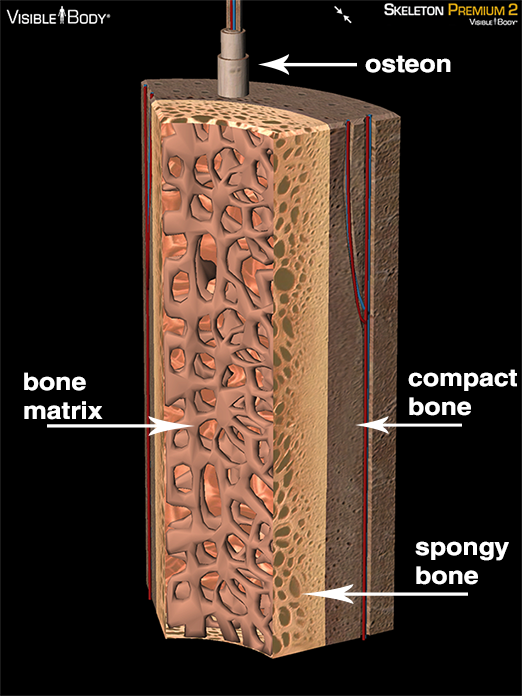
When tested for their differentiation abilities, the SJSCs made bone, cartilage and fat. Again, the age of the rat from which they had come from did not matter. SJSCs from aged rats differentiated just as well as SJSCs from younger animals. This is not the case for mesenchymal stem cells from older or younger rats. Mesenchymal stem cells from older rats differentiate rather poorly while those from younger rats differentiate rather well. Thus, these SJSCs are definitely a different kind of stem cell.
SJSCs also expressed a series of genes commonly found in active stem cells (telomerase and sirtuin 1). Such genes are normally not found in stem cells from older patients or older rats. Therefore, these cells may have anti-aging properties.
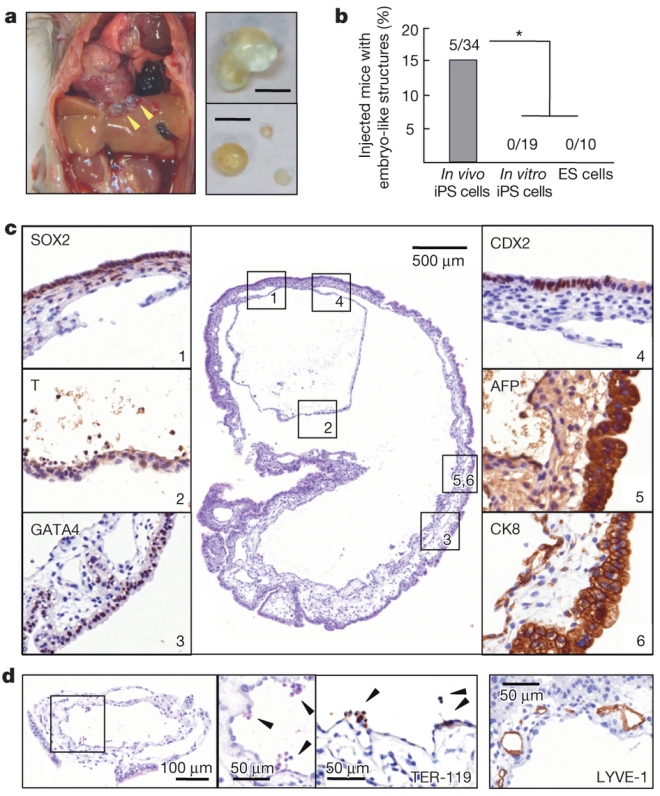
Ashraf wanted to test his SJSCs in action so he gave the rats some heart attacks and transplanted one million SJSCs into the ventricles of these rats. To compare the effects of the SJSCs, rat hearts were also injected with culture medium, whole bone marrow cells, and SJSCs from aged animals.
Animals injected with SJSCs from aged animals had smaller heart scars, a more normal echocardiogram, higher ejection fraction, greater heart muscle shortening, and lower end-diastolic and end-systolic volumes than the others. In short, the SJSCs helped heal the heart after a heart attack. The SJSCs also induced the formation of a whole host of new blood vessels in the heart.
Other experiments showed that SJSCs did not produce tumors when injected into nude mice.
In summary, the SJSCs possessed high proliferation and differentiation potential regardless of the age of the host animal. They also expressed genes commonly found in pluripotent cells, and also express genes relevant for cardiac differentiation, and anti-aging functions. The ends of the chromosomes were quite long and normal in SJSCs, which is something not seen in aged cells. FInally, SJSCs significantly reduced the size of the infarct in the heart after a heart attack and restored heart function.
Are SJSCs VSELs? I doubt it. The number of VSELs diminish with age, but Ashraf found just as many SJSCs in old mice as in young mice. Also, the proliferation and differentiation of capacity of VSELs decreases with age, but not for SJSCs. Thirdly, VSELs do not express CD90 whereas SJSCs do. Finally and probably most importantly, SJSCs were isolated from the mesenchymal stem cell population whereas VSELs come from the mononuclear fraction. These are two distinct cell populations and SJSCs come from an altogether different population of cells than VSELs. This seems to indicate that VSELs, if they exist, are not the same as SJSCs.
Ashraf writes in his paper: “… it is very important for the reproducibility of results by multiple laboratories to confirm the developmental potential of these pluripotent stem cells before considering their application in a clinical setting.” To that I can only say, “Amen and Amen.” Should Ashraf’s work be confirmed in other laboratories and should SJSCs be found in human bone marrow, they might make for a handy source of cells for regenerative medicine.