Within the heart resides a cell population called “c-kit cells,” which have the ability to proliferate when the heart is damaged. Several experiments and clinical trials from several labs have provided some evidence that these cells are the resident stem cell population in the heart that can repair the heart after an episode of cardiac injury.
Unfortunately, a few new studies, and in particular, one that was recently published in the journal Nature, seem to cast doubt on these results. Jeff Molkentin of Cincinnati Children’s Hospital Medical Center and his co-workers have used rather precise cell lineage tracing studies in mice to follow c-kit cells and their behavior after a heart attack. His results strongly suggest that c-kit cells rarely produce heart muscle cells, but they do readily differentiate into cardiac endothelium, which lines blood vessels.
“The conclusion I am led to from this is that the c-kit cell is not a cardiac stem cell, at least in term of its normal, in vivo role,” said Charles Murry, a heart regeneration researcher at the University of Washington who was not involved in this study.
Molkentin’s study is what some stem cells researchers are calling the nail in the coffin for c-kit cells. In fact the Molkentin paper is simply the latest in a series of papers that were unable to reproduce the results of others when it comes to c-kit cells. Worse still, one of the leading laboratories in the c-kit work, Piero Anversa at Harvard Medical School, has had to retract on of this papers and there is also some concern about his publication regarding the SCIPIO trial. Eduardo Marbán, an author of the new study and a cardiologist at the Cedars-Sinai Heart Institute in Los Angeles, said, “There’s been a tidal wave in the last few weeks of rising skepticism,” Nevertheless, the present dispute is not yet settled, and many scientists still regard the regenerative powers of c-kit cells as a firmly established fact.
In his laboratory, Piero Anversa and his colleagues and collaborators have shown that c-kit cells—cardiac progenitor cells expressing the cell surface protein c-kit—can produce new heart muscle cells (cardiomyocytes). Anversa and others also helped usher these cells, which are also known as CPCs or cardiac progenitor cells, into clinical trials to test whether they might help repair damaged cardiac tissue. This culminated in the SCIPIO trial, which showed that patients treated with their own CPCs showed long-lasting and remarkable improves in heart function.
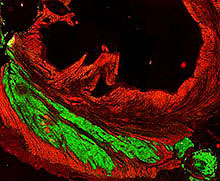
Follow-up work by other research teams, however, has not been able to confirm these studies, and their work has raised doubts about the potential of c-kit cells to actually build new heart muscle. In his contribution to the c-kit controversy, Molkentin and his colleagues genetically engineered mouse strains in which any c-kit-expressing cells and their progeny would glow green. To do this, they inserted a green fluorescent protein gene next to the c-Kit locus. Therefore any c-kit-expressing cells in the heart would not only glow green, but whatever cell type they differentiated into would also glow green. After inducing heart attacks in these mice, Molkentin and others discovered that only 0.027 percent of the heart muscle cells in the mouse heart originated from c-kit cells. “C-kit cells in the heart don’t like to make myocytes,” Molkentin told The Scientist. “We’re not saying anything that’s different” from groups that have not had success with c-kit cells in the past,” Molkentin continued, “we’re just saying we did it in a way that’s unequivocal.”
Molkentin’s study did not address why there’s a discrepancy between his results and those of Anversa and another leader in the c-kit field, Bernardo Nadal-Ginard, an honorary professor at King’s College London. Last year in a paper published in the journal Cell, Nadal-Ginard and his colleagues showed that heart regeneration in rodents relies on c-kit positive cells and that depleting these cells abolishes the regenerative capacity of the heart.
In an email to a popular science news publication known as The Scientist, Nadal-Ginard suggested that technical issues with Molkentin’s mouse model could have affected his results, causing too few c-kit cells to be labeled. Additionally, “the work presented by Molkentin used none of our experimental approaches; therefore, it is not possible to compare the results,” Nadal-Ginard said in an e-mail.
Anversa said his lab is working with the same mouse model Molkentin used, “but our data are too preliminary to make any specific comment. Time will tell.”
Molkentin’s paper seems point to further problems with Aversa’s work with c-kit cells. Last month, one of the papers Anvera and his group had published in the journal Circulation had to be retracted because the data used the write that paper were “sufficiently compromised.” Then a few days later, the paper describing the results of the SCIPIO study that appeared the journal The Lancet expressed concern about supplemental data that was included with the published results. These data came from the human clinical trial that treated heart patients with their own c-kit cells. Harvard Medical School and Brigham and Women’s Hospital are investigating what went wrong with this study and the publication itself.
Regardless of Anversa’s present tribulations, Marbán is advancing another type of heart-specific stem cell, called cardiosphere-derived cells or CDCs. Marbán and his colleagues have already used CDCs in a human clinical trial known as the CADUCEUS trial. In this trial, heart attack patients treated with CDCs saw their heart scars shrink. Marbán said he had been a true believer in c-kit cells, until the data started mounting against them. “The totality of the evidence now says the c-kit cell is no longer a cardiomyocyte progenitor,” he said.
Now even if c-kit cells do not make new heart muscle, it is possible that they heal the heart through other means. The patients in the SCIPIO trial saw real, genuine improvements in their heart function and these results cannot be so cavalierly dismissed. In fact, Murry said that just because the mechanistic basis for the human study remains in doubt, promising clinical results should not be dismissed. “Those results can be considered independent,” he said. Molkentin also added that it’s possible that c-kit cells work in unknown ways to repair heart tissue. Since clinical treatments involves high levels of c-kit cells that have been immersed in culture conditions, “Perhaps these cells act a little different,” Molkentin said.
Nadal-Ginard also noted that discrepancies do exist between his data and those of others, and that these discrepancies should not be papered over, but should be robustly debated and addressed. He said he’d be willing to work with Molkentin to get to the bottom of it. “The concept under dispute is too important for the field of regenerative medicine—and regenerative cardiology, in particular—to turn into a philosophical/dogmatic argument instead of settling it in a proper scientific manner.” Here here.



![(A) Scatterplot showing the natural relationship between scar size and left ventricular ejection fraction ∼5 months post-myocardial infarction (circles). Each cross symbol represents the mean values (at the intersection of the vertical and horizontal bars [obtained from all patients with magnetic resonance imaging measurements]), whereas the width of each bar equals ±SEM of scar size and left ventricular ejection fraction of CADUCEUS patients at baseline, 6 months, and 1 year; the crosses are superimposed onto the scatterplot showing prior data from post-myocardial infarction patients with variable scar sizes. The changes in left ventricular ejection fraction in CDC-treated subjects are consistent with the natural relationship between scar size and ejection fraction in convalescent myocardial infarction, whereas the changes in left ventricular ejection fraction in controls fall within the margins of variability. (B) Changes in end-diastolic volume from baseline to 1 year. (C) Changes in end-systolic volume from baseline to 1 year. CDCs = cardiosphere-derived cells; EDV = end-diastolic volume; EF = ejection fraction; ESV = end-systolic volume; LV = left ventricle.](https://beyondthedish.files.wordpress.com/2014/05/cdcs-heart-scar-size-vs-ef.jpg?w=147&h=300)