A research team from the Spanish National Cancer Research Center (CNIO) has shown that partial pharmacological inhibition of the PI3K enzyme in obese mice and monkeys reduces body weight and physiological manifestations of metabolic syndrome, specifically diabetes and hepatic steatosis (fatty liver disease), without any signs of side effects or toxicities. They published their work in the journal Cell Metabolism. This collaborative project between the Tumor Suppression Group headed by Manuel Serrano at the CNIO (Madrid, Spain) and the Translational Gerontology Branch headed by Rafael de Cabo at the U.S. National Institute on Aging, National Institutes of Health (NIH, Baltimore, MD, USA), included the participation of the NeurObesity group of CIMUS led by Miguel Lopez at the University of Santiago de Compostela (Santiago de Compostela, Spain).
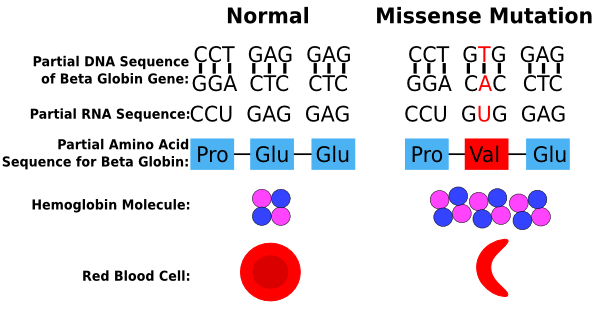
PI3K (phosphatidylinositol-3-kinase) is the name of an enzyme that regulates the balance between the biosynthesis of cellular components and the burning of nutrients to make energy in cells. Specifically, PI3K promotes cellular growth and biosynthesis, which can lead to the induction of growth and multiplication of cells, and ultimately could lead to cancer.
For this reason, scientists who investigate cancer have has a long-standing interest in designing pharmacological inhibitors of PIK3. CNIO, in fact, has developed its own experimental inhibitor, CNIO-PI3Ki, which is being studied for applications as a cancer treatment in combination with other compounds. As part of the characterization of the PI3K inhibitor and to understand how it affects the balance between the use and storage of nutrients in the body, the Serrano team decided to study the effects of CNIO-PI3Ki on metabolism.
“At this point we have veered away from the original anticancer aspects of these inhibitors. In our previous studies, we had seen that one of the normal physiological functions of the PI3K enzyme is to promote the storage of nutrients. We found this to be of particular interest because it is precisely this type of manipulation, regulation of the balance between storage and use of nutrients, that is sought after in treating obesity,” explains Ana Ortega-Molina, the first author of the study, who is working at the Memorial Sloan-Kettering Cancer Center in New York.
To test the effect of their PI3K inhibitor on metabolism, CNIO scientists administered small doses of the CNIO-PI3Ki inhibitor to obese mice for 5 months while those mice were fed a high-fat diet. During the first 50 days, the obese animals lost 20% of their body weight, at which point their weight stabilized. The treatment was administered for 5 months and during the whole time, these mice maintained a stable weight (20% below the weight of non-treated obese mice), despite continuing feeding with a high-fat diet. They also improved their pathological symptoms of diabetes (high glucose levels in the blood) and hepatic steatosis (fatty liver).
“When it comes to obesity, constant weight loss can be extremely dangerous. The ideal solution is to alter the balance between the use and storage of nutrients, to strike a new balance in which there is greater use and less storage,” explains Elena López-Guadamillas who, in collaboration with Ana Ortega-Molina, carried out most of the experimental work. This study showed that the drug had no side-effects and did not produce irreversible effects on metabolism, which is also desirable for its possible future use as a treatment in humans.
In non-obese animals that were fed a standard diet, the administration of the drug had no effect, which is another indication of its safety. “This shows that the activity of the PI3K enzyme is only relevant when there is an excess of nutrients, that is, a high-calorie or high-fat diet,” adds López-Guadamillas.
CNIO scientists then collaborated with the U.S. National Institutes of Health (NIH) in order to test the CNIO-PI3Ki compound on obese monkeys (macaques). They used a very low dose to ensure higher safety margins, but even with these very high doses, the daily treatment of these obese animals over a 3-month period reduced the total amount of fatty tissue by 7.5% and improved the symptoms of diabetes.
Obesity is one of the most important risk factors within the spectrum of serious diseases that constitute the metabolic syndrome. Many pharmacological agents have been discovered that lead to weight loss, but these drugs often have unacceptable toxic effects (partly due to the fact that these previous agents act on the brain centers that control appetite). In this respect, CNIO-PI3Ki seems to be the exception, at least in animal models thus far, as no such side-effects have been observed, even after long-term treatments (5 months in mice and 3 months in monkeys).
A series of safety characteristics that have been demonstrated in mice is shown below:
1) Selective: CNIO-PI3Ki only produces weight loss in mice that receive an excess of nutrients and not in mice that eat a normal balanced diet. This shows that PI3K plays an important role in the storage of nutrients when food intake is excessive, but is not so important under a normal diet.
2) Weight loss in the mice is due exclusively to loss of fatty tissue; no losses occur in other tissues such as liver, muscle or bone.
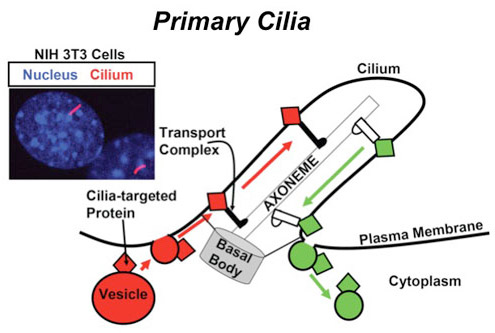
3) It does not affect the brain: CNIO-PI3Ki does not cross the blood-brain barrier.
4) It does not affect the hypothalamus: The hypothalamus is a specialized structure of the brain that is exceptional because it lacks a blood-brain barrier (a structure that controls the entrance of substances from the blood to the brain) and it controls many metabolic processes, including appetite and satiety. No effects on the main neuropeptides produced by the hypothalamus related to appetite and satiety have been noted in the mice. These last studies have been carried out in collaboration with the research group led by Miguel López at the University of Santiago de Compostela.
5) It works on a long-term basis: The effects of CNIO-PI3Ki were maintained over at least a 5-month period of treatment in mice, which suggests that resistance mechanisms are not developed. This is very important, as it is a common problem found in other compounds that affect metabolism.
6) Reversibility: The effects of CNIO-PI3Ki were reversible, which means that when the treatment was interrupted and a high-fat diet maintained, the mice regained weight. This indicates that CNIO-PI3Ki does not cause irreversible changes.
The next logical step, once the beneficial effects of CNIO-PI3Ki have been demonstrated in obese mice and monkeys, is to perform clinical trials on humans. “The leap from animals to humans is complex, expensive and full of uncertainties. Many treatments that are promising in animals turn out not to be effective in humans or toxicities appear that were not observed in animals. But, obviously, in spite of the uncertainties, we have to give it a try,” says Manuel Serrano. “Clinical trials require large investments and are undertaken with the aim of marketing a treatment. We are very optimistic about the possibility of entering into an agreement soon with a multinational pharmaceutical company interested in carrying out clinical trials with CNIO-PI3Ki to treat obesity and metabolic syndrome in humans,” says Serrano.