Scientists from the Columbia University Medical Center have succeeded in transforming human stem cells into functional lung and airway cells. This finding has significant potential for modeling lung disease, screening lung-specific drugs, and, hopefully, generating lung tissue for transplantation.
Study leader, Hans-Willem Snoeck, professor of medicine and affiliated with the Columbia Center for Translational Immunology and the Columbia Stem Cell Initiative, said, “Researchers have had relative success in turning human stem cells into heart cells, pancreatic beta cells, intestinal cells, liver cells, and nerve cells, raising all sorts of possibilities for regenerative medicine. Now, we are finally able to make lung and airway cells. This is important because lung transplants have a particularly poor prognosis. Although any clinical application is still many years away, we can begin thinking about making autologous lung transplants – that is, transplants that use a patient’s own skin cells to generate functional lung tissue.”
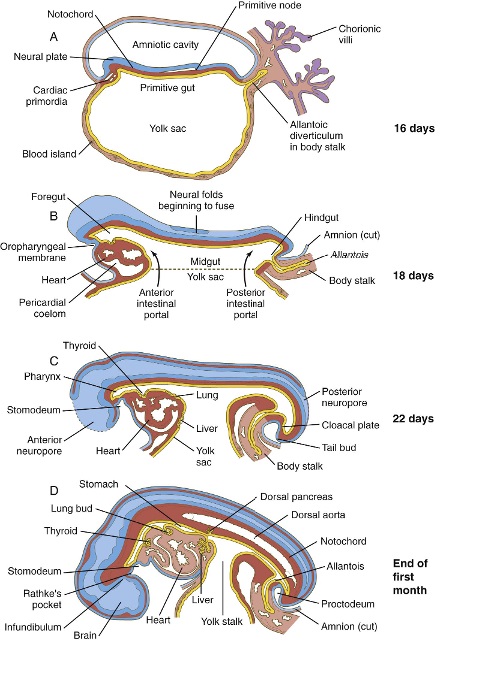
The research builds on Snoeck’s earlier discoveries in 2011 that a set of chemical factors could induce the differentiation of embryonic or induced pluripotent stem cells into “anterior foregut endoderm,” which is the embryo in the tissue from which the lungs form (Green MD, et al. Generation of anterior foregut endoderm from human embryonic and induced pluripotent stem cells. Nat Biotechnol. 2011 Mar;29(3):267-72).
In his new study, Snoeck and his colleagues found new factors that can transform anterior foregut endoderm cells into lung and airway cells. In particular, Snoeck and his co-workers were able to establish the presence of “type 2 alveolar epithelial cells,” which secrete the lung surfactant that maintains the lung alveoli (those tiny sacs in the lung where all the oxygen exchange takes place).
With these techniques, lung researchers hope to study diseases like idiopathic pulmonary fibrosis (IPF), in which type 2 epithelial cells seem to divide and produce scarring in the lungs.
“No one knows what causes the disease, and there’s no way to treat it,” said Snoeck. “Using this technology, researchers will finally be able to create laboratory models of IPF, study the disease at the molecular level, and screen drugs for possible treatments or cures. In the longer term, we hope to use this technology to make an autologous lung graft. This would entail taking a lung from a donor, removing all the lung cells, leaving only the lung scaffold; and seeding the scaffold with new lung cells derived from the patient. In this way, rejection problems could be avoided.”
Snoeck is investigating this approach in collaboration with researchers in the Columbia University Department of Biomedical Engineering.