If we take tissue samples from the mouth and grow them in the laboratory and manipulate them, we might be able to cure the blind. Blind people who suffer from stem cell deficiency in the cornea might be able to see again by using stem cells isolated from the mouth. Furthermore, this treatment might not only restore vision, but it might also ameliorate pain in the cornea.
Ophthalmologist Tor Paaske Utheim has conducted research for over ten years on how to cure certain types of blindness by using stem cells harvested from tissue obtained from different parts of the body. He then transplants this cultured tissue into the damaged eye, and patients who suffer from blindness as a result of corneal stem cell deficiencies can regain their sight. Recently, Utheim’s research has utilized stem cells from the mouth to grow new corneal tissue, and has also tried to design optimal methods to store and transport this tissue to treat patients.
Utheim is the head of a research group at the Faculty of Dentistry at the University of Oslo (UiO) and the Department of Medical Biochemistry at Oslo University Hospital.
Using cells extracted from the mucous membrane lining the inside of the mouth (the oral mucosa) can restore vision is new to most people. Only ten years ago, this was considered impossible, but results confirm the potential of this method. Twenty clinical studies from various countries have, to date, shown good results, according to Utheim. These clinical trials, however, have only applied these cells to a group of diseases caused by stem cell deficiency in the cornea.
Utheim and his colleagues hope to treat patients with eye injuries caused by so-called limbal stem cell deficiencies. This disorder can be caused by such things as UV radiation, chemical burns, serious infections like trachoma, and various other diseases, some of which are heritable. The number of people worldwide affected by limbal stem cell deficiency is unknown, but in India alone there is an estimated 1.5 million. This disorder most often affects people living in developing countries.
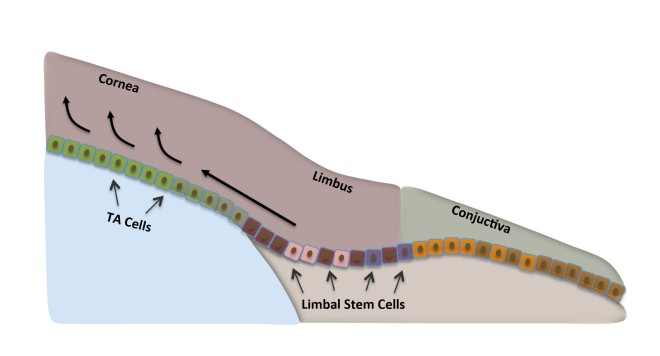
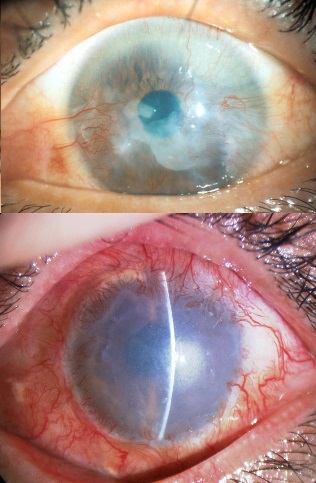
Stem cells that are found at the outer edge of the cornea help to keep the surface of the cornea even and clear. In limbal stem cell deficiencies, the stem cells have been damaged, and they cannot renew the cornea’s outermost layer. Instead, other cells grow over the cornea, which clouds the cornea. The cornea can become fully or partially covered, explains Utheim, which leads to impaired vision or blindness.
Others suffer from severe pain as well. When one patient was interviewed by Norwegian national broadcaster NRK about his limbal stem cell deficiency, he responded: “I don’t know what’s worse: the pain, or losing my sight.”
Utheim explained that when stem cells do not work properly, ulcers can develop in the cornea, which exposed nerve fibers. Since the number of nerve fibers is far higher in the cornea than for example in the skin, it is not surprising that some patients experience severe pain.
A breakthrough within the field occurred about ten years ago when Japanese researchers showed that cells from the oral mucosa could be used to replace limbal stem cells in patients with limbal stem cell deficiency. Although it had been possible since the late 1990s to cure the disorder using cultured stem cells. The available treatment relied on the patient having a healthy eye from which to collect cells.
Further developments made it possible to harvest cells from a relative or deceased individual, but using limbal stem cells from other patients required the use of strong immunosuppressive drugs for the patients, which could cause serious side effects.
A milestone seemed to be reached when it became possible to use a patient’s own cells to treat blindness in both eyes without the need for immunosuppressive drugs. Strangely, this makes some sense because there are similarities between the oral mucosae and the surface of the eye (see Utheim TP. Stem Cells. 2015;33:1685-1695). Originally, using mouth mucosal cells to treat the eye required that the laboratory where the cells are cultured and the clinic where the patients are treated be quite close together. Because there were no protocols for storing extracted oral mucosal cells so that they can be easily kept and transported. This has made the treatment virtually inaccessible to many of the patients who need it the most, namely those in developing countries. However, this may be about to change.
Utheim’s research group is now on the brink of a development that will make it possible to cure both severe pain and blindness in patients who are spread over a larger geographical area than before (see Islam R, et al. PLoS One. 2015;10:e0128306.). “Today, cells from the mouth are cultured for use in the treatment of blindness in only a few specialized centers in the world. By identifying the optimal conditions for storing and transporting the cultured tissue, we would allow for the treatment to be made available worldwide, and not just close to the cell culture centers,” said Rakibul Islam, who is a PhD candidate in the Department of Oral Biology at the Faculty of Dentistry.
Islam is collaborating with Harvard Medical School to introduce this method of treating blindness to clinics around the world. Islam’s findings could also help improve treatment outcomes. “Being able to store the cultured tissue in a small sealed container for a week increases the technique’s flexibility significantly. It makes it easier to plan the operation and allows for quality assurance through microbiological testing of the tissue before transplantation,” Islam explained.
One of the things that Islam and his colleagues have discovered is the specific temperature range at which cells from the mouth should ideally be stored at after culture. Islam has shown that cultured mouth stem cells retain their quintessential properties best between 12 and 16 degrees Celsius (See Dolgin, Elie. Nature Biotechnolgy, 2015;33:224-225.).
During a brief stint at Harvard University, Islam also examined which areas of the mouth are best suited to use in regenerative medicine. In other words, Islam and his colleagues wanted to know which parts of the mouth contain cell layers that regenerate the fastest. Islam explained this using this example: “If you burn any part of your mouth on hot coffee, it heals so quickly that by the next morning you have forgotten about it. This is because the oral mucosa contains cells that multiply quickly. We wanted to investigate whether there were regional differences in the mouth that we could exploit for the treatment of limbal stem cell deficiency.”
Islam continued, “Our results show that the location from which the mucosal tissue is harvested has a striking impact on the quality of the cultured tissue.”
The results from this particular study have not yet been published.
This research can potentially give hope to the many blind that live far away from centralized cell culture laboratories. In work by Utheim in 2010, in collaboration with the ophthalmologist Sten Ræder, he developed storage technology for cultured stem cells that enables the cultured tissue to be transported in a small custom-made plastic container. Tissue from stem cells is thus freed from expensive and bulky laboratory equipment and provides a whole new level of flexibility.
Utheim said “The sample of cells from the mouth can be sent by air over long distances to specialist laboratories with first-class equipment and expertise. After a couple of weeks of laboratory cultivation, the sender may receive the tissue back ready for use. An ophthalmologist could then transplant the stem cells onto the patient’s eye.”
However, the container was just one step in the right direction: “Now we have identified those areas of the mouth that may be best suited for regenerative medicine, and developed a method for storing and transporting tissue from centralized, highly specialized tissue culture centers to clinics worldwide. Our findings are helping to simplify and streamline the clinical procedures, and to make the treatment far more accessible than it is today,” said Islam, who admitted that the transport potential of the project has been integral to his own enthusiasm. He continued, “Although the scientific and technical aspects of our project are very exciting, it has been especially motivating to think of the possibilities this storage technology brings to treating blindness in all parts of the world, including my homeland Bangladesh.”
A central laboratory for the growth of stem cells already exists in Italy. In fact, earlier this year the European Medicines Agency approved the procedure for the cultivation of stem cells from the cornea in EU laboratories. This is the first stem cell therapy to be approved by the European Medicines Agency, according to the journal Nature Biotechnology. Utheim described the approval as an important step towards the implementation of stem cell technology over larger geographical areas. To date, almost 250 people with limbal stem cell deficiency have undergone treatment involving transplantation of stem cells grown from their own mouth cells. “This provides a good basis for judging the success of the treatment” Utheim says.
He has recently published an article in the journal Stem Cells on the inherent potential of cells from the mouth to regenerative medicine. Roughly three out of four treatments are described as successful.




