New preclinical experiments by scientists at the University of Pennsylvania have established that genetically engineered T-cells can drive severe autoimmune diseases into remission without suppressing the patient’s immune system. If the principles applied in this study also prove to be true in human patients, they can potentially revolutionize the treatment of autoimmune diseases.
Autoimmune diseases result when your immune system recognizes your own cells and tissues as foreign and mounts and immune response against them. Autoimmune diseases like systemic lupus erythematosus (also known as “lupus”), rheumatoid arthritis, scleroderma, multiple sclerosis, celiac disease, Sjögren’s syndrome, polymyalgia rheumatic, or ankylosing spondylitis can deeply affect the health of an individual and can also cause large amounts of tissue damage.
Treatment of autoimmune diseases usually requires high doses of drugs that suppress the immune system, such as corticosteroids, or various types of biological agents that also cause a host of undesirable side effects.
This new study, however, by scientists from the Perelman School of Medicine at the University of Pennsylvania have adapted an already-existing technology to remove the subset of antibody-making cells that cause the autoimmune disease. This strategy removes the rogue immune cells without harming the rest of the immune system.
In these experiments, the University of Pennsylvania team examined an autoimmune disease called pemphigus vulgaris or PV. PV results when the immune system recognizes a protein called desmoglein-3 (Dsg3) as foreign and attacks it. Dsg3 helps form attachment sites called “desmosomes” that normally adhere skin cells together to form tight, tough sheets. Desmosomes are also found between epithelial cells, myocardial cells, and other cell types.
Current therapies for autoimmune diseases like PV use drugs like prednisone and rituximab, which suppress large parts of the immune system. Consequently, prednisone and rituximab can leave patients vulnerable to potentially fatal opportunistic infections and cancers.
To treat PV, University of Pennsylvania researcher Aimee Payne and her colleagues used a mouse version of PV that is fatal in mice. Their experimental treatment, however, successfully treated this otherwise fatal autoimmune disease without causing any unintended side effects, which might harm healthy tissue. The results from these experiments were published in the journal Science.
“This is a powerful strategy for targeting just autoimmune cells and sparing the good immune cells that protect us from infection,” said Dr Payne, who serves as the Albert M. Kligman Associate Professor of Dermatology at the Perelman School of Medicine.
In collaboration with Dr. Michael Milone, assistant professor of Pathology and Laboratory Medicine, Payne and her colleagues adapted the Chimeric Antigen Receptor T-Cell (CART-Cell) technology that is being successfully used to experimentally treat malignant cells in certain leukemias and lymphomas. “Our study effectively opens up the application of this anti-cancer technology to the treatment of a much wider range of diseases, including autoimmunity and transplant rejection,” Milone said.

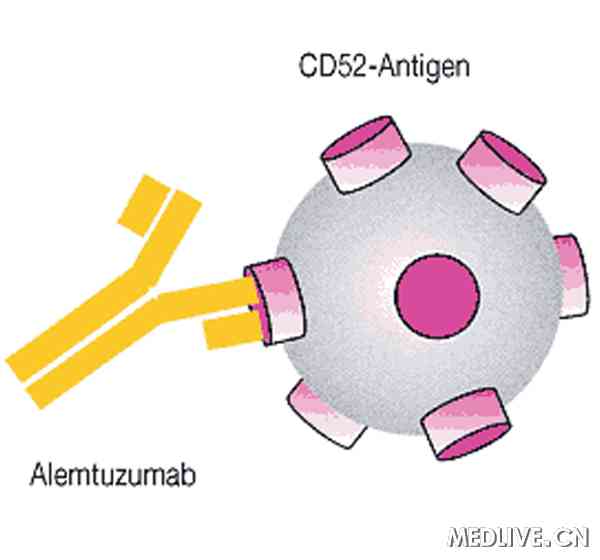
CART-Cells are T-lymphocytes that have been extracted from the peripheral blood of cancer patients and then genetically engineered to express a receptor that specifically recognizes a protein on the surface of tumor cells. These chimeric antigen receptor (CAR)-expressing cytotoxic T-lymphocytes have the ability to recognize and destroy tumor cells, which shrinks the tumor and potentially cures the patient.
The core concepts behind CAR T-cells were first described in the late 1980s. Unfortunately, technical challenges prevented the development of this technology until later. However, since 2011, experimental CAR T cell treatments for B cell leukemias and lymphomas have been successful in some patients for whom all standard therapies had failed.
Antibody-producing B-lymphocytes or B-cells can also cause autoimmunity. A few years ago, a postdoctoral researcher in Payne’s laboratory named Dr. Christoph T. Ellebrecht came upon CAR T cell technology as a potential strategy for deleting rogue B-cells that make antibodies against a patient’s own tissues. Soon Payne and her team had teamed up with Milone’s, which studies CAR T cell technology. Their goal was to find a new way to treat autoimmune diseases.
“We thought we could adapt this technology that’s really good at killing all B cells in the body to target specifically the B cells that make antibodies that cause autoimmune disease,” said Milone.
“Targeting just the cells that cause autoimmunity has been the ultimate goal for therapy in this field,” noted Payne.
Because an excellent mouse model existed for PV, Payne and Milone decided to examine pemphigus vulgaris. Since PV consists of a patient’s antibodies attacking those molecules that normally keep skin cells together, it can cause extensive skin blistering and is almost always fatal. PV is treatable with broadly immunosuppressive drugs such as prednisone, mycophenolate mofetil, and rituximab.
However, to treat PV without causing broad immunosuppression, the Penn team designed an artificial CAR-type receptor that would home the patient’s own genetically engineered T-cells exclusively to those B-cells that produce harmful anti-Dsg3 antibodies.
Payne and Milone and their colleagues developed a “chimeric autoantibody receptor,” or CAAR, that displays fragments of the Dsg3 on their cell surfaces. Since the Dsg3 protein is the target of the PV-causing B-cells, the CAAR acts as a lure for the rogue B cells that target Dsg3. The CAAR effectively brings the cells into fatal contact with the therapeutic T cells.
After testing a battery of different cultured, genetically engineered T-cells, these teams eventually found a CAAR that worked well in cell culture and enabled host T cells to efficiently destroy anti-desmoglein-producing B-cells. These cultured cells worked so well that they even killed B-cells isolated from PV patients. The engineered CAAR T cells also performed successfully in a mouse model of PV. The CAAR T-cell effectively killed desmoglein-specific B cells, prevented blistering, and other manifestations of autoimmunity in the animals. “We were able to show that the treatment killed all the Dsg3-specific B cells, a proof of concept that this approach works,” Payne said.
Not only were these treatments devoid of undesirable side effects in the laboratory mice they studied, but they maintained their potency despite the presence of high levels of anti-Dsg3 antibodies that might have swamped out their CAARs.
Next, Payne plans to test her treatment in dogs, which can also develop PV and often die from it. “If we can use this technology to cure PV safely in dogs, it would be a breakthrough for veterinary medicine, and would hopefully pave the way for trials of this therapy in human pemphigus patients,” Payne said.
Penn scientists would also like to develop applications of CAAR T cell technology for other types of autoimmunity. Organ transplant rejection, which is also related to autoimmunity, complicates organ transplants, and normally requires long-term immunosuppressive drug therapy, may also be treatable with CAAR T cell technology.
“If you can identify a specific marker of a B cell that you want to target, then in principle this strategy can work,” Payne said.


![Structures of opsins and of the chromophore retinal. (a) A model of the secondary structure of bovine rhodopsin. Amino-acid residues that are highly conserved in the whole opsin family are shown with a gray background. The retinal-binding site (K296) and the counterion position (E113) are marked with bold circles, as is E181, the counterion in opsins other than the vertebrate visual and non-visual ones. C110 and C187 form a disulfide bond. (b) The chemical structures of the 11-cis and all-trans forms of retinal. (c) The crystal structure of bovine rhodopsin (Protein DataBank ID: 1U19 [PDB:1U19]). The chromophore 11-cis-retinal, K296 and E113 are shown in stick representation in the ringed area. (d) The structure of the Schiff base linkage formed by retinal within the bovine opsin, together with the counterion that stabilizes it.](https://beyondthedish.files.wordpress.com/2015/08/opsins.jpg?w=660)